 |
| Foto : boditech.co.kr |
D-dimer is a mixture of cross-linked fibrin degradation products, which is formed after fibrin clots are degraded by a fibrinolytic enzyme called plasmin. D-dimer reflects global activation of platelet coagulation pathway and the degree of thrombin turnover (1, 2). Thus, D-dimer levels have been the most popularly used parameter for the frontline assessment of suspected deep vein thrombosis (DVT) or pulmonary embolism (PE) for almost 30 years (3, 4). In general, commercial D-dimer assays for blood show a high sensitivity up to 95% but have poor specificity, making it difficult to prove the presence of DVT or PE instead of another clotting complication.
Additionally, elevated levels of D-dimer have been reported in pregnancy, cancer, inflammation, surgery, the elderly, and remain a confounding factor limiting its use (5–9). However, the negative predictive values are nearly 100% accurate, with negative D-dimer test results of indication of a lack of DVT or PE. Hence, the main clinical application of D-dimer assay is to safely rule out DVT, PE, or disseminated intravascular coagulation (10, 11).
Among the commercially available assay systems for D-dimer, enzyme-linked fluorescence (FL) immunoassays and microlatex immunoturbidimetric assays are popularly used (12, 13). Although their performances satisfy the requirements for D-dimer assays in terms of high diagnostic sensitivity and negative predictive values, these assays have some limitations in application during emergency situations or in analyzing a single sample (14, 15).
Thus, we aimed to develop a new D-dimer assay that was out DVT, PE, or disseminated intravascular coagulation (10, 11).
Among the commercially available assay systems for D-dimer, enzyme-linked fluorescence (FL) immunoassays and microlatex immunoturbidimetric assays are popularly used (12, 13). Although their performances satisfy the requirements for D-dimer assays in terms of high diagnostic sensitivity and negative predictive values, these assays have some limitations in application during emergency situations or in analyzing a single sample (14, 15).
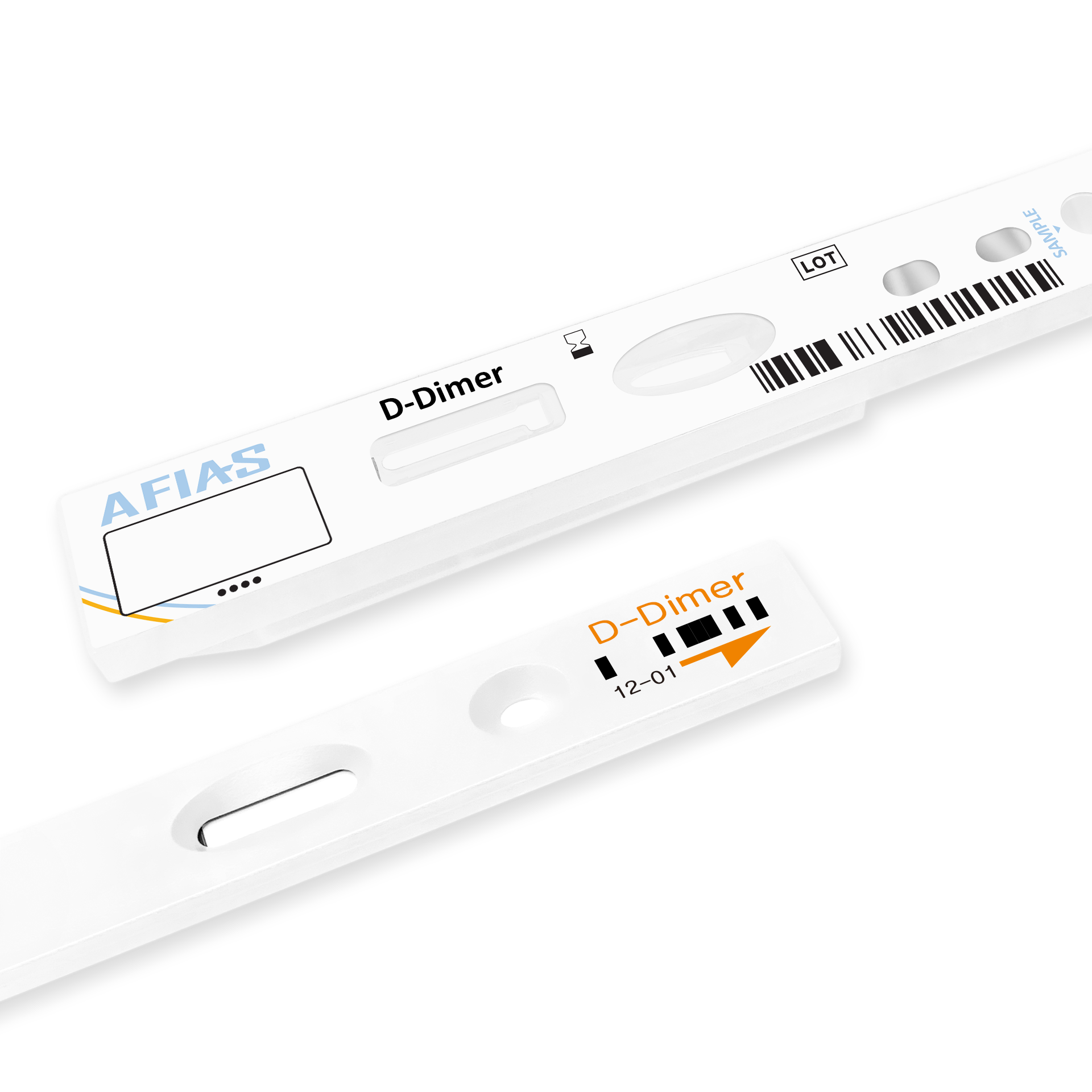
Thus, we aimed to develop a new D-dimer assay that was cost-effective and reliable, and could work with whole blood on a point-of-care test (POCT) platform. Here, we introduce a new D-dimer assay system that provides results in 12 min, has a POCT platform, and a reliable analytical performance compared to automated reference analyzers. This newly developed D-dimer assay system takes advantage of a simple lateral flow immunochromatographic assay (ICA) basis, adds a sandwich-type antibody scheme, and employs FL dye as a tracer to detect the level of D-dimer in samples. The FL-ICA D-dimer assay system consists of a monoclonal antibody coated (mAb) strip in a disposable cartridge, a detection buffer containing FL-labeled mAb, and biotin-bovine serum albumin (BSA), a chip for the calibration curve, and a laser FL scanner.
MATERIALS AND METHODS
Materials
Human D-dimer and mAb were purchased from Hytest Ltd. (Turku, Finland), and both streptavidin and biotin– BSA were purchased from Sigma-Aldrich (St. Louis, MO). Sephadex G25 and activated Alexa Fluor 647 were obtained from Amersham Pharmacia Biotech (Piscataway, NJ) and Molecular Probes (Eugene, OR), respectively. Nitrocellulose membrane (NC) was purchased from Millipore (Watertown, MA), sample pad and the absorption pads were obtained from Schleicher and Schuell (Keene, NH).
Labeling of Antibodies With Fluorescent Dye
For conjugation of the anti-D-dimer-mAb with a FLdye, 10 μl of a 1 mol/l sodium bicarbonate buffer (pH 8.3) was mixed with 100 μl of anti-D-dimer-mAb (1 mg/l) in phosphate-buffered saline (PBS) and followed by the addition of 1 μl of activated Alexa Fluor 647 (10 g/l) to the mixture. After overnight incubation at 4◦C, the mixture was applied onto a Sephadex G25 column to remove the free dye, and FL-labeled mAb conjugates were collected as elutes after centrifugation of the column at 2,500 rpm for 2 min. The biotin–BSA complex was similarly conjugated with Alexa Fluor 647, and FL-labeled biotin–BSA conjugates were purified with same processes as noted above, and used as an internal control for the assay system. The FL-labeled mAb and the FL-labeled biotin–BSA were mixed together with the assay buffer to form the detection buffer and were kept at 4◦C until use.
